Winter is commonly associated with respiratory viruses such as cold and flu. But each winter, thousands of people’s lives are put at risk as their symptoms are disregarded or confused with the flu, when in actual fact they have sepsis.
Sepsis is one of the biggest killers in the world, associated with one in five deaths worldwide. In the UK, around 245,000 people develop sepsis each year, leading to 48,000 deaths. To put these figures into context, sepsis kills significantly more people than breast, bowel and prostate cancer combined.
Yet many people – health professionals included – continue to overlook the symptoms and underestimate the severe consequences that failure to treat sepsis promptly can have. Delays to treatment for sepsis are a common cause of legal claims for compensation. Every hour that treatment is delayed, the risk of death increases by 7.6 percent.
Hospitals are complex environments and emergency departments have been pushed to their limits during the coronavirus pandemic. Staff have been forced to prioritise patients presenting at A&E and the quality of care patients are receiving has been compromised.
However, Canadian researchers are pioneering a new technique using AI technology to rapidly detect sepsis early. But will automation and machine learning improve the frightening mortality rate of sepsis and reduce the risk of life-changing complications in survivors?

Clinical negligence issues around sepsis
The first few hours after a patient presents at hospital are critical to ensure the timely administration of emergency antibiotics to fight the cause of infection. Ideally, antibiotic treatment should start within an hour of diagnosis to reduce the risk of serious complications or death.
Yet failure to diagnose and/or rapidly treat sepsis are the leading causes of sepsis clinical negligence claims. But for this delay to urgent treatment, some patients who died of sepsis would have survived.
Other failures might include:
- Incorrect diagnosis
- Failure to recognise early signs
- Delayed referral to hospital by GP
- Failure to take timely history/examination
- Not completing necessary tests to identify the source of infection
- Lack of regular monitoring
These could be due to various issues within the medical setting, such as inadequate staff training, time constraints, disorganised handovers etc. The winter months in particular add impossible pressures to an already overstretched and overworked NHS. But there is still a duty of care to keep patients safe and ensure a reasonable standard of care.
With sepsis, the condition can deteriorate rapidly and, even with all the right treatment, the rate of survival can be low. However, the Canadian research led by The University of British Columbia has found that using artificial intelligence can identify sets of genes that predict whether a patient will acquire severe sepsis when a person first arrives for medical care. From this, tests can be developed to allow healthcare providers to quickly identify the body’s dysfunctional response to an infection by measuring specific gene-expression biomarkers associated with the disease.
How is sepsis currently managed?
NHS trusts should follow the National Early Warning Signs (NEWS) parameters to diagnose sepsis in patients.
The NEWS parameters measure:
- Respiratory rate
- Oxygen saturation
- Systolic blood pressure
- Pulse rate
- Level of consciousness
- Temperature
The UK Sepsis Trust recommends that any adult who is unwell or has a NEWS score of more than five should be assessed for sepsis, using red flag criteria to prioritise those at highest risk. The National Institute for Health and Care Excellence (NICE) also recommends ambulance services pre-alert hospitals when any high risk criteria are present.
But sepsis isn’t always easy to spot, and some situations may be clinically challenging. Many of the possible symptoms are vague or similar to less threatening conditions such as the flu or chest infection. Improvements must be made to prevent so many tragic cases of people dying unnecessarily from overwhelmingly severe sepsis.
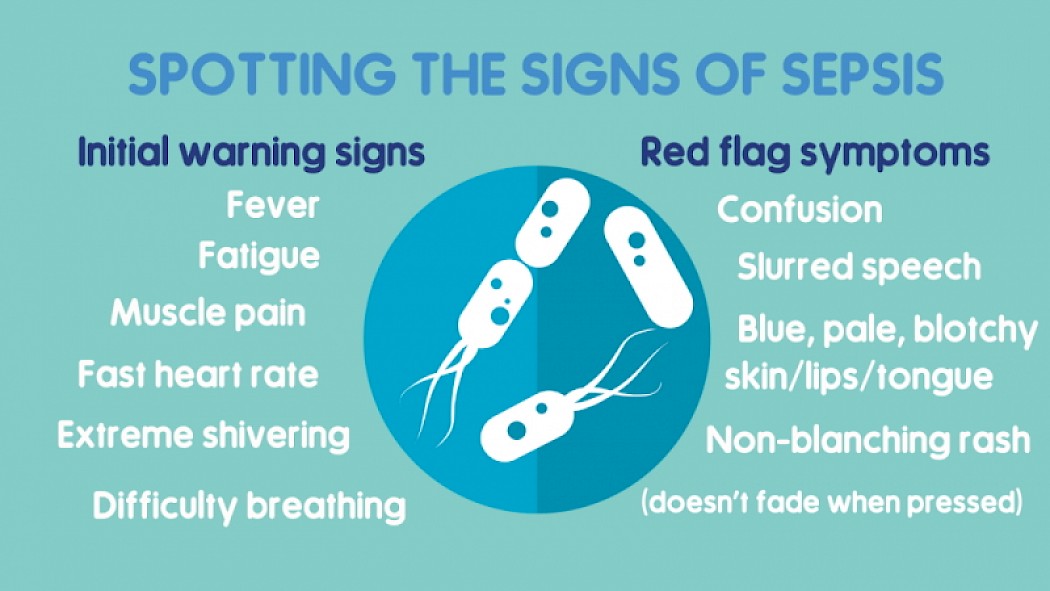
Signs and symptoms of sepsis
Families affected by sepsis will be all too familiar with what it is and the devestating impact it can have on lives. But for those who don't here are a few questions about sepsis answered.
What is sepsis?
The terms sepsis, septicaemia, and blood poisoning are often used interchangeably. However, while they have similar symptoms, strictly speaking sepsis and septicaemia are separate illnesses with different diagnoses. Septicaemia is when bacteria/infection enters the bloodstream, leading to the term blood poisoning. If left untreated, septicaemia can lead to sepsis.
Sepsis is when the body’s immune system overreacts to the bacteria/infection, resulting in inflammation throughout the body. When this inflammation occurs with extremely low blood pressure, a patient is said to go into septic shock, which is where the medical emergency arises.
It’s important to point out that only a small percentage of people with sepsis will become critically ill.
What are the complications of sepsis?
Severe sepsis can cause abnormal blood clots which damage tissues within the body and can lead to organ failure, necrotising fasciitis (flesh-eating disease), amputation, and death.
The death rate for sepsis is high. In survivors, 40 percent will suffer permanent, life-changing after-effects and disabilities such as PTSD, cognitive impairment, chronic pain, organ dysfunction
What causes sepsis?
Sepsis is triggered by an infection which sends the immune system into overdrive. This can be almost any infection.
Bacterial infections are the most common cause of sepsis, such as pneumonia, peritonitis caused by a perforated bowel, dental infections, urinary tract infections, MRSA, open wounds, or infections at catheter sites. In newborn babies, Group B strep contracted from the mother at birth is a leading cause of sepsis and meningitis.
However, you can also develop sepsis from viral infections such as the common cold, flu, Covid-19, HIV, or chickenpox. It can also be caused by parasitic infection (i.e., malaria, tapeworm)
Who is at risk of sepsis?
Because sepsis is triggered by an infection, anyone can contract it at any point in their life. However, there are some groups of people who are more susceptible:
- Babies under 1
- Over 75s
- People with diabetes
- People with a weakened immune system, i.e., chemotherapy, leukaemia organ transplant
- People who have recently given birth, had a miscarriage or abortion
- People who have recently had surgery
- People who are prone to infection
How is sepsis treated?
It is imperative that antibiotics are administered to treat the bacterial infection within one hour of a patient presenting at hospital. Other treatments that may be necessary, dependent on the severity of the infection, include fluids to prevent dehydration and kidney failure, the use of a ventilator to help breathing, blood thinners if clots have occurred, or surgery to remove the infection such as an abscess or gangrene.