A 50-year-old widow who lost her husband due to failures before and during cardiac surgery received £715,000 in compensation. Before his death in April 2015, the claimant (C) had cared for her husband for almost two years while he was in a persistent vegetative state. This was due to lack of oxygen to the brain caused by undiagnosed fluid around his heart following surgery.
The deceased first began feeling unwell in 2013 when investigations found a type B1 thymoma, a large growth between his lungs with node involvement. He was referred for consideration for surgery to remove the thymoma from his chest cavity.
However, he had previously had blood clots in both his legs and had an inferior vena cava (IVC) filter fitted and was taking warfarin blood thinners long-term. Before the scheduled surgery, the surgical team asked him to stop taking warfarin and instead prescribed heparin injections to use in the days before surgery.
His pre-operative aPTT results, which checks how long the blood takes to clot, came back abnormal (prolonged) and it was alleged that this should have been further investigated to determine the underlying cause. From this, either corrective methods should have been used, or surgery deferred.
But the surgery went ahead as planned two days later.
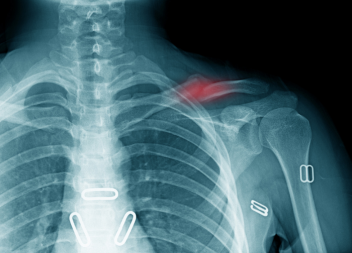
Due to the position of the tumour, which had become fixed to a major vein in the chest, surgical removal left a large raw space between his lungs. Surgeons were also unaware of his prolonged aPTT which increased his risk of post-surgical bleeding. A small, single drain was fitted which was inadequate and became easily blocked.
The deceased lost 350ml of blood during surgery, an amount well in excess of what should be expected during surgery of that nature. Blood loss was controlled with a haemostatic gauze which, again, would not normally be required. The drain had to stay in post-surgery, but it had been inserted too high in the chest, so it was more likely to become blocked or not drain properly particularly when he sat up in bed.
Back on the ward, the deceased complained of not feeling right and having a fear something was wrong. His wife also complained to the nursing team of his visible signs of deterioration, but these were not acted upon.
In the early hours of the morning, the deceased underwent emergency surgery for cardiac tamponade, where blood or fluids fill the space between the sac that encases the heart and the heart muscle. Due to the extreme pressure on his heart, he went into cardiac arrest and his brain was starved of oxygen.
Sadly, he never regained full consciousness and was in a near persistent vegetative state. He could sense his family and friends in the room and was minimally aware of his surroundings, but had no chance of improvement. He remained in a near persistent vegetative state for 23 months, during which time his wife and three children visited the hospital daily to care for him.
He died in April 2015 from pneumonia and sepsis brought on by his injuries almost two years earlier.
After her husband’s death, his widow sought the help of Caroline Moore at Medical Solicitors to bring a clinical negligence claim against the defendant NHS trust for failures in pre-operative haematological care, as well as in the performance of the surgery itself.
The majority of the £715,000 compensation received was for financial losses, including the statutory bereavement award for his widow. He left behind the couple’s three children, two of whom still lived at home, who all received damages for the loss of the parental love and affection. However, £150,000 of the award was compensation for the pain, injury and suffering of the deceased throughout the long period of being in an apparent minimally aware coma prior to his sad death.