The widow of a 58-year-old man who died of oesophageal cancer after being negligently discharged from surveillance for Barrett’s oesophagus has been awarded £540,000 in compensation.
The deceased had been having regular endoscopic surveillance for almost eight years after being diagnosed with Barrett’s mucosa with focal high-grade dysplasia (abnormal cell changes) in 2005. However, due to misinterpreted findings and a lack of knowledge of his medical history by a junior doctor, he was wrongly discharged in 2013 after a Barrett’s mucosa was mistaken for a hiatus hernia.
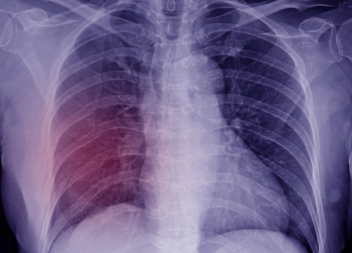
By the time cancer was diagnosed in 2017, it had already spread to the deceased’s bones, liver and lungs. With palliative chemotherapy the only treatment option available, he was given a year to live but managed to live a further four years before he passed away in Woking Hospice in September 2020.
Before his death, he suffered deteriorating health and was admitted to hospital numerous times for various invasive procedures. Amongst other GI related conditions, he was treated for slowly enlarging tumours on his liver, persistent bile duct obstruction, biliary sepsis, a collapsed lung, fluid on both lungs, and mineral deficiencies.
As per the deceased’s wishes, Matthew Brown recovered compensation after his death to maximise the benefit to his family, with the majority of the claim for past and future loss of financial and services dependency.
The Defendant, Royal Surrey County Hospital NHS Foundation Trust, admitted breach of duty occurred when the deceased was discharged in 2013. But for this mistake, he would have returned for surveillance two years later and his cancer diagnosed at an earlier stage. On the balance of probabilities, the cancer would have been treatable.
Barrett’s oesophagus is a rare pre-cancerous condition where the normal cells in the lining of the oesophagus change to resemble the lining of the intestine. Patients with Barrett’s oesophagus are at an increased risk of developing oesophageal cancer and should undergo regular surveillance via an endoscope to pick up cell changes (dysplasia).
After the deceased’s dysplasia was diagnosed in 2005, he was placed on six-monthly reviews. By 2007, biopsies taken showed the cells in his oesophagus had changed to become more like those in the intestine. His reviews changed to two-yearly. At the end of 2008, a 7cm Barrett’s oesophagus was detected and in 2011 no sinister features were found.
At his next review in 2013, it was reported he had a 7cm hiatus hernia, where the stomach extends from the abdomen to the chest; he was discharged with no need for future follow-ups.
However, three and a half years later he went to his GP complaining of trouble swallowing. A large, ulcerated lesion was found in his oesophagus as well as another lesion in the fundus at the top of his stomach. Biopsies and a PET scan confirmed this was a gastro-oesophageal adenocarcinoma and that it had metastasised around his body.
Investigations revealed that the junior doctor who reviewed the deceased in 2013 was not aware of his previous history of high-grade dysplasia. They also misinterpreted the findings; what they thought was a 7cm hiatus hernia was likely a 3cm Barrett’s mucosa and 4cm hernia. As a result of this, no biopsy was taken and there was no recall plan for on-going surveillance.
Throughout the case, Matthew worked with experts in the fields of upper GI surgery and oncology. The final settlement of £540,000 was reached out of court in July 2021 which included general damages at £75,000, bereavement award of £15,120, loss of earnings of £120,000, care and assistance of £80,000, past and future loss of financial and services dependency of £417,000 and further miscellaneous losses and expenses.